What are the parathyroids?
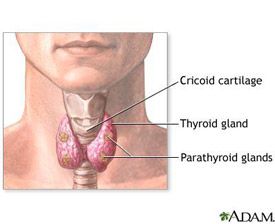
The parathyroids are four tiny glands in your neck, two on each side of your thyroid gland. They make parathyroid hormone (PTH) which controls the level of calcium in the blood. Calcium is very important for the normal functioning of muscles, nerves, and bones. It is absorbed through the intestines and stored in the bones. Parathyroid hormone raises blood levels of calcium by increasing intestinal absorption of calcium, and by dissolving calcium from the bone into the bloodstream.
What is hyperparathyroidism?
Some people make too much parathyroid hormone, a condition called hyperparathyroidism. This condition is most common in middle-aged and older women, but can occur in men or women at any age, and can run in families. In 8 of 10 patients with hyperparathyroidism, the cause is a single benign tumour. In two of 10, more than one parathyroid gland is enlarged. Cancer is rare. The overactive parathyroid steals calcium from your bones and puts it into the bloodstream. The kidneys try to clear the excess calcium and can form stones. High blood calcium can cause you to feel tired and irritable, and have aches and pains in bones, muscles, and joints. Over time, your bones can become weak, and your risk of broken bones is higher.
What are the symptoms of hyperparathyroidism?
- Weak bones, called osteoporosis, which can lead to fractures
- Kidney stones, poor kidney function
- High blood pressure
- Abdominal pain
- Increased thirst and frequency of urination
- Constipation
- Stomach ulcers and pancreatitis
- Psychiatric problems
- Arrythmias and heart disease
- Difficult to control blood sugar in diabetics
- Weakness and fatigue, loss of energy
- Memory and concentration problems
- Muscle and joint aches and pains
- Abdominal and back pains
- Feeling “older” than you should
- Mood swings or depression
- Headaches
- Poor sexual function
- Itchy skin
IMPORTANT*** These vague symptoms improve in 85% of patients after successful parathyroid surgery. Bone density also improves, reducing the risk of fractures.***
Treatment of hyperparathyroidism
The only effective treatment for hyperparathyroidism is surgery to remove the overactive gland(s). In the hands of an experienced endocrine surgeon, surgery can cure the condition in 98% of cases. There is no effective non-surgical treatment for hyperparathyroidism. Before surgery, you will have a parathyroid CT scan or a sestamibi scan (a painless scanning test) and a neck ultrasound to see if there is one enlarged gland that can be located.. If the abnormal gland is seen, you can have “parathyroid mini-surgery” though a very small incision, and go home the next morning.
If the enlarged gland is not seen on scanning, you should still consult with an expert parathyroid surgeon. The operation is slightly longer, but is still successful in 95% of cases. The surgery takes less than an hour. You will be completely asleep during the operation, and will feel no pain. Recovery is quick, with most patients going home the next day, and feeling very little discomfort. Most are back at work in a about a week.
Frequently Asked Questions
Is there any other treatment besides surgery?
No. Surgery is the only effective treatment of hyperparathyroidism.
What if I don't have the surgery?
Even if you think you have no symptoms, you may feel much better after you are cured. If you don’t have surgery, you will continue to have high blood calcium, and many symptoms listed above. Without surgery, your bones will continue to become weaker, and possibly break. There is evidence of increased risk of high blood pressure, stroke, heart disease, and even shorter life expectancy, from untreated hyperparathyroidism.
What are the possible complications of parathyroid surgery?
The nerves that control your voice are closely associated with the parathyroid glands. Temporary voice changes are common, but usually resolve within weeks to months. In 1 in 100 parathyroid operations, the nerve that controls the voice may permanently affected, leaving your voice hoarse. Some patients have difficulty with projection of the voice and production of high pitched sounds. This problem is more common, and may affect your singing voice. “Voice fatigue” may occur as well.
Sometimes the surgery will not cure the hyperparathyroidism. In the hands of an experienced endocrine surgeon, failure to cure occurs in roughly 2 in 100 patients. The most common reason is another enlarged parathyroid that was not seen on initial imaging. These can be found at a second operation, required in about 2% of patients. Sometimes the normal parathyroid glands become “lazy” because the abnormal gland was doing all the work. They may take some time to recover, so some patients require extra calcium tablets on a temporary basis. Rarely, after a bilateral parathyroid exploration, the parathyroids do not recover, and calcium and vitamin D may be needed on a permanent basis. Occasionally, the tumour can recur. I recommend an annual calcium blood test after parathyroid surgery.
There is a small risk of bleeding into the wound. If this happens, it may be necessary to have a second operation to evacuate the blood so it does not interfere with your breathing. Infection is relatively uncommon, and is easy to treat should it occur.
WHAT ARE THE RISKS OF PARATHYROID SURGERY?
As with anything in life, there are risks to surgery. These risks are weighed against the risks of not having surgery. Listed below are some of the possible complications of surgery. Risks include, but are not limited to:
- Permanent voice hoarseness - 1%
- Failure to cure the hyperparathyroidism - 2%
- Permanent hypoparathyroidism - ½ % (0% for mini-surgery)
- Infection of Incision - Less than 1%
- Haematoma or Bleeding - Less than 1%
- Seroma (fluid collection) - 1% (temporary)
- Swelling and black/blue - 5-10% (temporary)
- Keloid or overgrown scar - uncommon in Caucasians, 10-20% in Asians, Indians, Africans
- Scar tethering/tightness - 5% early, usually settles with time
- Other unforeseen risks
You will require general anaesthetic, given by a specialist anaesthetist. I work with a select group of outstanding anaesthetists. Risk of a serious complication in a healthy person is very rare. Potential risks include, but are not limited to:
- Heart problems (death, heart attack, arrhythmias)
- Lung problems (pneumonia, wheezing)
- Blood clots (stroke, clots in leg veins or lungs)
- Drug reactions (also possible with local anaesthetic)
- Chipped teeth
- Other unforeseen risks
You will meet the anaesthetist just before your operation and have the chance to discuss these further. If you would like to see the anaesthetist before the day of surgery, an appointment can be arranged.
How long will I be hospitalized?
Most patients are admitted to the hospital on the morning of their surgery. If you have mini parathyroid surgery, you may be able to go home that same evening, depending on how you feel. If you don’t feel well enough to go home, you live alone or far away, your surgery was late in the day, or if you’ve had the traditional parathyroid surgery, you will be able to go home the next day.
What type of anesthesia will I have?
You will have a general anesthesia. You will be completely asleep during the operation. You will have local anaesthesia injected into the neck (cervical plexus block) to make you even more comfortable when you wake up. This local anaesthetic block will probably leave your ear lobes numb for 24 hours as well.
When will I know the results of the surgery?
The calcium levels generally return to normal within 12-48 hours of surgery.
Will I have a scar?
Yes. All surgery causes a scar, and how a patient scars is dependent on the individual. Techniques I use to minimize scarring include careful incision placement in a natural skin crease, and hypoallergenic suture material (to avoid inflammation). In patients prone to keloids, In patients prone to keloids, I use skin glue rather than sutures. The glue eventually flakes off by itself.
For parathyroid “mini-surgery,” the scar is about 1-1 1/2 inches (2.5-3.5cm). If you need a full neck exploration, it will be bigger (5-6cm). As a general rule, no matter which operation you need, it is unusual to have a very noticeable scar after six months. Scars continue to fade for three years.
Will I have pain after the operation?
Most patients are surprised at how comfortable they are after parathyroid surgery. Although you should be able to eat and drink normally, the main complaint is sore throat and discomfort with swallowing for 1-2 days. You may also have a headache, or pain at the back of your neck. Most patients take Panadol and/or Nurofen to keep them comfortable at home. You can have a prescription for something stronger for the first few days in case you need it, but beware prescription pain medicine can make you drowsy and constipated, so do not drive, drink lots of water and eat plenty of fruits and vegetables.
Will I have stitches?
You will have stitches on the inside that dissolve on their own. You will have a waterproof Comfeel dressing so that you can shower or bathe as usual (but do not submerge the incision for 5 days). Leave the dressing in place until your first post-operative visit, where it will be removed. It can stay in place up to four weeks.
Will I have any physical restrictions after my surgery?
Your activity level depends on the amount of discomfort you experience. Many patients have resumed golf or tennis within a week after the operation. Most patients return to work in a week, and you are able to drive as soon as your head can be turned comfortably without prescription pain pills (this limitation is for driver safety).
PREPARATION for SURGERY
Medications and Fasting
- Please shower at home the evening before or the morning of surgery
- For morning surgery, Do Not Eat anything after midnight the night before surgery unless otherwise instructed. You may drink clear liquids until one hour before your admission time. Clear liquids include black coffee, tea, water, clear broth or apple juice. No milk or other cloudy liquids. Medication with a small sip of water is OK. Your surgery may be cancelled if you do not follow these instructions.
- For afternoon surgery, a light breakfast BEFORE 7AM is OK, and clear liquids only after that, until one hour before your admission time. Clear liquids include black coffee, tea, water, clear broth or apple juice. No milk or other cloudy liquids. Your surgery may be cancelled if you do not follow these instructions.
- Do Not Drink Alcoholic beverages 24 hours prior to your surgery.
- Do Not Smoke for 4 weeks before surgery or your risk of serious complications increases.
- Please take heart, blood pressure, cholesterol, and reflux medicines as directed with a sip of water. For insulin or diabetic medications, please check with your anaesthestist.
- Diabetic SGLT2i medications MUST be stopped for 48 hours. This includes anything ending in “FLOZIN” (empagliflozin, ertugliflozin, canagliflozin, dapagliflozin) and brand names Invokana, Farxiga, Xigduo, Qtern, Jardiance, Synjardy, Steglatro, Segluromet, Stegluhan, and Glyxambi.
- Blood thinners: Stop aspirin or warfarin 5-7 days prior to surgery. Cease rivaroxaban (Xarelto) at least 24 hours before. Cease apixaban (Eliquis) at least 48 hours before. Discuss with your prescribing doctor if you need bridging injectable blood thinners.
- Do Not bring valuables such as money, jewelry etc. Do not wear make-up.
- Bring toiletries and loose fitting, comfortable clothing to wear upon discharge.
- You will be required to remove contact lenses, jewelry, dentures, and wigs.
- Arrange for a responsible adult to drive you home after discharge.
- Notify us if there is a change in your condition prior to surgery (such as a cold, cough, fever or infection). If severe, your surgery may need to be postponed for your safety.
- Stop all herbal medications 4 weeks before surgery unless discussed beforehand. Especially Fish oil, Ginseng, Garlic, and Gingko, St. John’s Wort, or Tumeric, which increase the risk of bleeding.
THE DAY of YOUR SURGERY
- On the day of your surgery, report to hospital reception at the appointed time.
- If you have not already done so, you will meet your anaesthetist.
- You may need a blood test or ECG prior to surgery.
- After the operation, you spend will some time in the recovery room before going to the ward.
- On the day of discharge, you are not permitted to:
- Drive a Car nor operate power equipment.
- Drink Alcoholic Beverages.
- Sign important papers.
The above are not permitted on the day of surgery, nor while taking any prescription pain medication. Instructions regarding safe resumption of the above activities will be provided by your surgeon.
Post-Operative Instructions for Parathyroid Surgery.
Questions: call the office on .
Below are general instructions for patients who have had thyroid or parathyroid surgery. Since individual circumstances may vary, it is important that you discuss your individual post operative care with us.
Monitoring Your Progress
You should feel improvement every day after surgery. If you have any questions regarding your progress, call our office. You should make a follow up appointment approximately 1-2 weeks after your surgery.
Incision Care
Your incision is covered with a waterproof protective dressing. You can shower and wash your hair as usual, but do not soak or scrub the dressing. After showering, pat dry. Your dressing will be removed at your first post-operative visit. If you experience itching once the dressing is off, you may apply lotion to the scar. I recommend keeping Micropore tape on the scar (available at any pharmacy – it comes in brown or white – I think the brown looks better) for about 6 weeks. It will help the scar fade more quickly. Change it every few days, when it comes off on its own. Keep your neck and the scar moving by turning your head from side to side, tilting your head, and massaging your scar several times per day (with the tape in place).
You might notice bruising around your incision or upper chest and slight swelling behind the scar when you are upright. In addition, the scar may become pink and hard. This hardening will peak at about 3 weeks and may result in some tightness or difficulty swallowing, which will disappear over the next 3 to 4 months. You will also notice some numbness of the skin of your neck. This will gradually improve over time. Occasionally, patients get tethering of the scar on the inside, resulting in a tight feeling when swallowing or tilting the head back. If you experience this tightness, continue to stretch your neck and massage your scar firmly, several times per day. Turn your head back and forth and roll your shoulders to reduce stiffness. The tightness should settle down over time, usually by 3 months, but it continues to improve for three years.
Pain
The main complaint following parathyroid surgery is discomfort with swallowing. Some people experience a dull ache, while others feel a sharp pain. This should not keep you from eating anything you want, but the pain can be annoying for a day or two. Nurofen and/ or Panadol is generally enough to control this pain. Some people prefer Panadeine, but in general, stronger medications are not necessary for long. You may feel like you have phlegm in your throat. This is usually because there was a tube in your windpipe while you were asleep that caused irritation that you perceive as phlegm. You will notice that if you cough, very little phlegm will come up. This should clear up in 4 to 5 days. In a small proportion of patients, the “lump in throat” feeling persists for a few months, but in most cases is will eventually resolve.
Voice Changes
Your voice may go through some temporary changes with fluctuations in volume and clarity (hoarseness). Temporary changes are quite common. Generally, it will be better in the mornings and "tire" toward the end of the day. This can last for variable periods of time, but should clear in 4-6 months at most. There is a small (1/100) risk of permanent hoarseness. There is a higher chance your singing voice will be affected.
Hypocalcemia and Bone Health
Your bones have been starved of calcium during the time you have had hyperparathyroidism, and will now have the chance to grow strong again. After successful parathyroid surgery, I recommend you take three serves per day of calcium rich foods, or Caltrate two tablets daily (available at any chemist) to promote healthy bones. In addition to these supplements, an exercise routine using weights is also recommended In a small number of patients who have parathyroid surgery, the remaining parathyroid glands have become lazy, and do not function properly immediately after surgery. It is very rare after the mini-surgery, but about 5% if you need both sides of the neck explored. This is usually temporary and causes the blood calcium level to drop below normal (hypocalcaemia). Symptoms of hypocalcaemia include numbness and tingling in your hands, soles of your feet and around your lips. Some patients experience a "crawling" sensation in the skin, muscle cramps or headaches. These symptoms appear between 24 and 48 hours after surgery. It is rare for them to appear after 72 hours.
Hypocalcaemia is treated with extra calcium tablets. You can purchase Calcium (Caltrate) tablets over the counter. If you feel you need it, take two extra tablets (there is no danger in taking it, even if you do not need it.) The symptoms of tingling/numbness should improve within 30-45 minutes of taking the tablets. If they do not disappear, take two more, and repeat as necessary each 30-45 minutes. If the symptoms do not disappear after 3 doses, call my office in business hours, or after hours report to your nearest hospital emergency room to have your blood calcium checked. Some patients also need a tablet called calcitriol to help absorb calcium from your diet.
You should repeat the dose whenever the symptoms return. This may mean that you are taking as many as 2 tablets every 3 hours. It is important that you keep us informed. The hypocalcaemia should disappear over a few weeks. Keep a record and let us know at your post-surgery visit if you are needing extra calcium.
CONTACT MY OFFICE for any of the following symptoms:
- Fever >38.3 or chills.
- Increasing pain or redness around incision.
- Difficulty breathing.
- Tingling around the lips or fingertips not relieved by extra calcium tablets.
- Severe muscle cramps.
AN IMPORTANT WORD ABOUT THE COSTS OF TREATMENT
Insurance rebates have not kept pace with the cost of running a medical practice. As a consequence, there will be a gap to pay for the surgical fee and for the anaesthetist. Your insurance company might also charge you an excess for a hospital admission. We will advise you about expected out-of pocket costs not covered by insurance. If these costs represent an undue hardship for you, please discuss them with us.
ASK YOUR DOCTOR
We are here to help you. If you have any questions, please ask. It is often helpful to bring a family member with you to a consultation, or to write questions down so you won’t forget them.
