Prof. JULIE MILLER, BA, MD, FRACSSpecialist Endocrine Surgeon
(Including information from the SAGES - Society of American Gastrointenstinal and Laparoscopic Surgeons)
What are the adrenal glands?
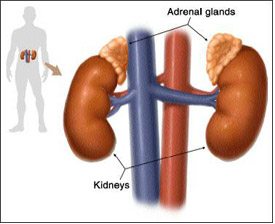
The adrenal glands are shaped like small pyramids and sit just above your kidneys, under the lower ribs at the back. They make many important hormones that control various bodily functions including adrenaline for the “fight or flight” response, cortisol, a “stress hormone,” and aldosterone, to help control your body’s salt levels and blood pressure. The adrenals also make a small fraction of the body’s sex hormones.
Tumours commonly form on the adrenal glands, but most of them are harmless and do not need to be removed. However, in some cases it is recommended to remove an adrenal tumour. Below are the most common reasons:
- To see if there is cancer: if there are features suspicious for cancer, like size >4cm or a certain appearance on imaging. Fortunately, malignant adrenal tumours are rare. Because they behave aggressively, though, there is a low threshold to remove any mass with suspicious features.
- Functioning Tumours - if the tumour is making too much of a hormone, like adrenaline (pheochromocytoma), cortisol (Cushing’s syndrome), or aldosterone (Conn’s syndrome.)
- Solitary Metastasis - if the adrenal tumour is a metastasis from another cancer, and it is the only location the cancer has spread.
- Cushing's disease with failed pituitary surgery sometimes your doctor may recommend removal of both adrenals if a pituitary tumour is making them overproduce cortisol and pituitary surgery has failed.
Frequently Asked Questions
How is an an adrenal tumour removed??
A general anaesthetic is required, so you will be fully asleep. There are 3 main approaches to Adrenal surgery:
OPEN: a large open incision is the procedure of choice for a very large tumour or a known adrenal cancer
LAPAROSCOPIC ANTERIOR: Keyhole surgery through the abdominal cavity has smaller incisions and a quicker recovery than open surgery. It is a safe approach for benign (non-cancerous) tumours <8-10cm.
PRA - POSTERIOR RETROPERITONEOSCOPIC ADRENALECTOMY: This technique is an improvement over the laparoscopic technique, as it causes less pain than even laparoscopic surgery, is safe in obese patients, and is not affected by scar tissue from previous abdominal surgery. PRA is safe for benign tumours <7cm. In fact, two thirds of patients require nothing more than panadol to relieve discomfort after PRA!
The patient is placed face down and the adrenal tumour removed via 3 small incisions in the back, just below the ribcage. The technique was developed in Europe by Prof. Martin Walz, and more than 2000 adrenal operations have been safely completed this way. Dr. Miller learned the procedure directly form Dr. Walz and was the first surgeon in Victoria (and the second in Australia) to perform it. As of early 2020, she has performed more PRA operations than any other surgeon in Australia, and has mentored more than ten surgeons in four states successfully perform PRA.
What are the potential complications of Adrenal surgery?
As with anything in life, there are risks to surgery. These risks are weighed against the risks of not having surgery. Listed below are some of the possible complications of surgery.
The rate of major complications after PRA is less than 2%.
Risks include, but are not limited to:
- Numbness or weakness of the flank muscles around the incision (usually temporary.)
- High blood pressure.
- Bleeding.
- Injury to surrounding organs such as the bowel, or the liver on the right or the spleen or pancreas on the left.
- Infection of the incisions.
- Bruising/swelling.
- Incisional hernia (less common with PRA or laparoscopic surgery).
- Collapsed lung (pneumothorax).
- Other unforeseen risks.
You will meet the anaesthetist just before your operation and have the chance to ask any additional questions.
- Heart problems (death, heart attack, arrhythmias)
- Lung problems (pneumonia, wheezing)
- Blood clots (stroke, clots in leg veins or lungs)
- Drug reactions (also possible with local anaesthetic)
- Chipped teeth
- Other unforeseen risks
You will meet the anaesthetist before your operation and have the chance to ask any additional questions.
What are the symptoms of adrenal gland tumours?
Patients with adrenal gland tumours may have no symptoms at all. A variety of symptoms can result from excess hormone production by the abnormal gland. Adrenal tumours associated with excess hormone production include pheochromocytomas, aldosterone-producing tumours, and cortisol-producing tumours. Typical features are described below.
- Pheochromocytomas produce excess hormones that can cause episodes of very high blood pressure and periodic spells characterised by severe headaches, excessive sweating, anxiety, palpitations, and rapid heart rate that may last from a few seconds to several minutes. These episodes can result in life-threatening strokes or heart attacks.
- Aldosterone producing tumours cause high blood pressure and low serum (blood) potassium levels. In some patients this may result in symptoms of weakness, fatigue, and frequent urination.
- Cortisol producing tumours cause a syndrome termed Cushing's syndrome that can be characterised by obesity (especially of the face and trunk), high blood sugar, high blood pressure, menstrual irregularities, fragile skin, and prominent stretch marks. Most cases of Cushing’s syndrome, however, are caused by small pituitary tumours and are not treated by adrenal gland removal. Overall, adrenal tumours account for about 20% of cases of Cushing’s syndrome.
- An incidentally found mass in the adrenal may be any of the above types of tumours, or may produce no hormones at all. Most incidentally found adrenal masses do not make excess hormones, cause no symptoms, are benign, and do not need to be removed. Surgical removal of incidentally discovered adrenal tumours is indicated if:
- The tumour is found to make excess hormones
- Is large in size (more than 4 cm in diameter)
- If there is a suspicion that the tumour could be malignant
- Adrenal gland cancers (adrenal cortical cancer) are rare tumours that are usually very large at the time of diagnosis. Removal of these tumours is usually done by open adrenal surgery.
If an adrenal tumour is suspected based on symptoms or has been identified by CT or other scan, the patient should undergo blood and urine tests to determine if the tumour is over-producing hormones. Special tests, such as a CT scan, nuclear medicine scan, MRI, or selective venous sampling may be used to obtain more information about the adrenal tumour.
How exactly is PRA performed?
- The surgery is performed under a general anesthesia, so you are asleep during the procedure.
- 3 small incisions are made in the back and small ports (metal tubes) are placed through them. The space above the kidney is filled with carbon dioxide gas so the surgeon can see
- A laparoscope (a small telescope) connected to a special camera is inserted through the port. This gives the surgeon a magnified view of your internal organs on a television screen.
- Your surgeon delicately separates the adrenal gland from its attachments and seals the blood vessels. Once the adrenal gland has been dissected free, it is placed in a small bag and is then removed through one of the incisions. This incision may need to be enlarged slightly to remove the tumour. The small incisions are then closed
What happens if the procedure cannot be performed by PRA?
In a small number of patients the PRA method cannot be performed. The operation is then converted to a laparoscopic or open procedure. Factors that may increase the possibility of choosing or converting to the "open" procedure may include:
- Large tumour size or very large patient size
- A history of prior abdominal surgery causing dense scar tissue (this affects laparoscopy but not PRA)
- Inability to visualise the adrenal gland clearly
- Bleeding during the operation
The decision to perform the open procedure is a judgment decision made by your surgeon either before or during the actual operation. When the surgeon feels that it is safest to convert to an open procedure, this is not a complication, but rather sound surgical judgment. The decision to convert to an open procedure is based strictly on patient safety.
What should I expect after Adrenal surgery?
After the operation, it is important to follow your doctor's instructions. Although many people feel better in just a few days, remember that your body needs time to heal. You should expect a one night stay in hospital, unless your medical condition requires that you stay longer.
- After adrenal gland removal, most patients can be cared for in a surgical ward. Occasionally, a patient with a pheochromocytoma may go to an intensive care unit after surgery to monitor blood pressure.
- Patients with an aldosterone-producing tumour will need a serum potassium level checked after surgery and may need to continue to take medications to control their blood pressure.
- Patients with cortisol-producing tumours and Cushing’s syndrome will need to take prednisone or cortisol pills after surgery. The dose is then tapered over time as the remaining normal adrenal gland resumes adequate production of cortisol hormone.
Will I have pain after the PRA operation?
Most patients are surprised at how comfortable they are after PRA surgery. You should be able to eat and drink normally, walk up and down stairs, and do light activity. Most patients take Panadol and/or Nurofen to keep them comfortable at home. You will have a prescription for something stronger for the first few days in case you need it, but beware prescription pain medicine can make you drowsy and constipated, so do not drive or operate heavy machinery, and drink lots of water and eat plenty of fruits and vegetables.
How long will I be hospitalised?
Most patients are admitted to the hospital on the morning of surgery and go home the next day unless your medical condition requires you to stay longer.
When will I know the findings of the surgery?
A final pathology report requires careful study of the surgical specimen. Therefore, the final report is usually not available until about one week after the operation.
Will I have stitches?
You will have stitches on the inside that dissolve on their own. You will have a waterproof Comfeel dressing so that you can shower or bathe as usual (but do not submerge the incision for 5 days). Leave the dressing in place until your first post-operative visit, where it will be removed.
Will I have any physical restrictions after my surgery?
In general, your activity level depends on the amount of discomfort you experience. Many patients have resumed golf or tennis within a week or two after the operation. Most patients return to work in a week, and you are able to drive as soon as you are comfortable. Let your body be your guide and use your common sense.
Preparation for Surgery
- Preoperative preparation includes blood tests, medical evaluation, and an ECG depending on your age and medical condition.
- After your surgeon reviews with you the potential risks and benefits of the operation, you will be asked to provide written consent for surgery.
- Patients with a pheochromocytoma will need special medications prior to surgery to control their blood pressure.
- Patients with an aldosterone-producing tumour may need to take extra potassium.
- Patients with Cushing’s syndrome will need to receive extra doses of cortisone medication on the day of surgery and for up to one year afterwards until the remaining adrenal gland has resumed normal function.
Medications and Fasting
- Please shower at home the evening before or the morning of surgery
- For morning surgery, Do Not Eat anything after midnight the night before surgery unless otherwise instructed. You may drink clear liquids until one hour before your admission time. Clear liquids include black coffee, tea, water, clear broth or apple juice. No milk or other cloudy liquids. Medication with a small sip of water is OK. Your surgery may be cancelled if you do not follow these instructions.
- For afternoon surgery, a light breakfast BEFORE 7AM is OK, and clear liquids only after that, until one hour before your admission time. Clear liquids include black coffee, tea, water, clear broth or apple juice. No milk or other cloudy liquids. Your surgery may be cancelled if you do not follow these instructions.
- Do Not Drink Alcoholic beverages 24 hours prior to your surgery.
- Do Not Smoke for 4 weeks before surgery or your risk of serious complications increases.
- Please take heart, blood pressure, cholesterol, and reflux medicines as directed with a sip of water. For insulin or diabetic medications, please check with your anaesthestist.
- Diabetic SGLT2i medications MUST be stopped for 48 hours. This includes anything ending in “FLOZIN” (empagliflozin, ertugliflozin, canagliflozin, dapagliflozin) and brand names Invokana, Farxiga, Xigduo, Qtern, Jardiance, Synjardy, Steglatro, Segluromet, Stegluhan, and Glyxambi.
- Blood thinners: Stop aspirin or warfarin 5-7 days prior to surgery. Cease rivaroxaban (Xarelto) at least 24 hours before. Cease apixaban (Eliquis) at least 48 hours before. Discuss with your prescribing doctor if you need bridging injectable blood thinners.
- Do Not bring valuables such as money, jewelry etc. Do not wear make-up.
- Bring toiletries and loose fitting, comfortable clothing to wear upon discharge.
- You will be required to remove contact lenses, jewelry, dentures, and wigs.
- Arrange for a responsible adult to drive you home after discharge.
- Notify us if there is a change in your condition prior to surgery (such as a cold, cough, fever or infection). If severe, your surgery may need to be postponed for your safety.
- Stop all herbal medications 4 weeks before surgery unless discussed beforehand. Especially Fish oil, Ginseng, Garlic, and Gingko, St. John’s Wort, or Tumeric, which increase the risk of bleeding.
The Day of Your Surgery
- On the day of your surgery, report to hospital reception at the appointed time.
- If you have not already done so, you will meet your anaesthetist.
- You may need a blood test or ECG prior to surgery.
- After the operation, you spend will some time in the recovery room before going to the ward.
- On the day of discharge, you are not permitted to:
- Drive a Car nor operate power equipment.
- Drink Alcoholic Beverages.
- Sign important papers.
The above are not permitted on the day of surgery, nor while taking any prescription pain medication. Instructions regarding safe resumption of the above activities will be provided by your surgeon.
Post-Operative Instructions for Adrenal Surgery
Questions: call the office on
Below are general instructions for patients who have had adrenal surgery. Since individual circumstances may vary, it is important that you discuss your individual post operative care with us.
Monitoring Your Progress
You should feel improvement every day after surgery. If you have any questions regarding your progress, call my office. You should make a follow up appointment approximately 2 weeks after your surgery.
Incision
Your incision is covered with a waterproof protective dressing. You can shower and pat dry as usual, but do not soak or scrub the dressing. Your dressing will be removed at your first post-operative visit. If you experience itching once the dressing is off, you may apply lotion to the scar. You might notice bruising around your incision. In addition, the scar may become pink and hard. This hardening is temporary and will last some weeks. You may also notice some numbness around the incision, pain or muscle laxity around your abdomen. This will gradually improve over time.
Pain
The main complaint following minimally invasive adrenal surgery is minor wound discomfort. Some people experience a dull ache, while others feel a sharp pain. This should not keep you from light activity. Nurofen and/ or Panadol is generally enough to control this pain. Stronger medications are not necessary for long.
Contact My Office for any of the following symptoms:
- Persistent fever >38.5 or chills.
- Persistent nausea or vomiting, unable to keep liquids down.
- Increasing pain or redness around incision.
- Persistent cough, shortness of breath, or difficulty breathing.
- Fainting or increased abdominal swelling.
An Important Word About the Costs of Treatment
Insurance rebates have not kept pace with the cost of running a medical practice. As a consequence, there will be a gap to pay for the surgical fee and for the anaesthetist. Your insurance company might also charge you an excess for a hospital admission. We will advise you about expected out-of pocket costs not covered by insurance. If these costs represent an undue hardship for you, please discuss them with us.
Ask Your Doctor
We are here to help you. If you have any questions, please ask. It is often helpful to bring a family member with you to a consultation, or to write questions down so you won’t forget them.
